Health
T-DXd Outperforms T-DM1 in HER2+ Breast Cancer Study
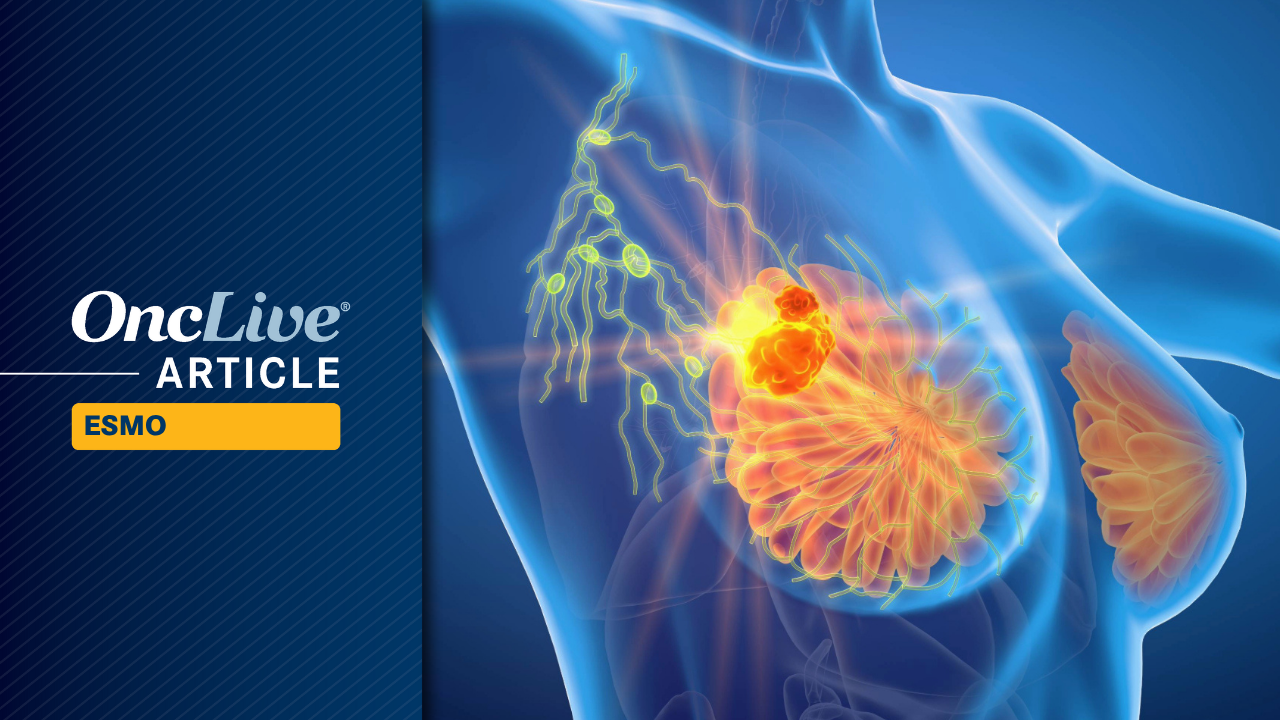
Patients with high-risk, HER2-positive breast cancer have shown significant improvement in invasive disease-free survival (IDFS) when treated with fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu) compared to ado-trastuzumab emtansine (T-DM1; Kadcyla). This finding, derived from an interim analysis of the phase 3 DESTINY-Breast05 trial, was presented at the 2025 ESMO Congress.
The trial involved a total of 1,635 patients, with those receiving T-DXd (n = 818) experiencing a 53% reduction in the risk of invasive disease or death compared to those treated with T-DM1 (n = 817). The hazard ratio was calculated at 0.47 (95% CI, 0.34-0.66; P < .0001). Three-year IDFS rates were reported as 92.4% for T-DXd and 83.7% for T-DM1.
Dr. Charles E. Geyer Jr., a professor of medicine and chief of the Division of Malignant Hematology and Medical Oncology at the University of Pittsburgh Medical Center, emphasized the broad applicability of T-DXd. He noted that patients benefited from this treatment regardless of various factors including age, hormone receptor status, and previous therapy regimens.
Historically, the phase 3 KATHERINE trial indicated that T-DM1 improved IDFS with a hazard ratio of 0.50 (95% CI, 0.39-0.64; P < .0001) and overall survival (OS) with a hazard ratio of 0.66 (95% CI, 0.51-0.87; P = .0027) for patients with HER2-positive early breast cancer. Despite these positive results, the data indicated unmet needs for more effective post-neoadjuvant treatments, particularly for patients with advanced locoregional disease.
The DESTINY-Breast05 trial was designed as a global, multicenter, randomized, open-label study. Participants were required to have residual invasive disease in the breast or axillary lymph nodes following neoadjuvant chemotherapy combined with a HER2-directed therapy. High-risk disease was defined as either inoperable early breast cancer or operable early breast cancer with axillary node-positive disease. All patients had centrally confirmed HER2-positive status and an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1.
Participants were assigned to receive either intravenous (IV) T-DXd at 5.4 mg/kg or IV T-DM1 at 3.6 mg/kg, both administered every three weeks for 14 cycles. The primary endpoint of the trial was IDFS, while disease-free survival (DFS) served as a key secondary endpoint. Other secondary endpoints included OS, distant recurrence-free interval (DRFI), and brain metastasis-free interval (BMFI).
In terms of patient outcomes, the T-DXd group had a median study duration of 29.9 months, with 72.3% of patients completing the study treatment, despite a 27.7% discontinuation rate primarily due to adverse effects. Conversely, in the T-DM1 group, the median study duration was 29.7 months, with 76.3% completing the treatment and a 23.7% discontinuation rate.
Adverse events (AEs) were reported in both treatment arms, with any-grade treatment-emergent AEs (TEAEs) observed in 99.5% of patients receiving T-DXd and 98.4% for T-DM1. Notably, serious TEAEs occurred in 17.4% of the T-DXd cohort compared to 13.6% in the T-DM1 group. The most common AEs for T-DXd included nausea (71.3%), constipation (32.0%), and decreased neutrophil counts (31.6%), while T-DM1 reported similar rates for nausea (29.3%) and fatigue (20.2%).
The findings from this trial indicate that T-DXd offers superior efficacy in managing high-risk, HER2-positive early breast cancer with residual invasive disease after neoadjuvant therapy, suggesting it could establish a new standard of care in this setting. Dr. Geyer concluded, “Adjuvant T-DXd demonstrated superior efficacy with manageable safety.”
Dr. Geyer disclosed receiving grants and contracts from multiple pharmaceutical companies, including Daiichi Sankyo and AstraZeneca, as well as support for the presentation from these organizations.
-
 Science4 weeks ago
Science4 weeks agoALMA Discovers Companion Orbiting Giant Red Star π 1 Gruis
-

 Politics2 months ago
Politics2 months agoSEVENTEEN’s Mingyu Faces Backlash Over Alcohol Incident at Concert
-

 Top Stories2 months ago
Top Stories2 months agoNew ‘Star Trek: Voyager’ Game Demo Released, Players Test Limits
-

 World2 months ago
World2 months agoGlobal Air Forces Ranked by Annual Defense Budgets in 2025
-

 World2 months ago
World2 months agoMass Production of F-35 Fighter Jet Drives Down Costs
-
 World2 months ago
World2 months agoElectrification Challenges Demand Advanced Multiphysics Modeling
-

 Business2 months ago
Business2 months agoGold Investment Surge: Top Mutual Funds and ETF Alternatives
-
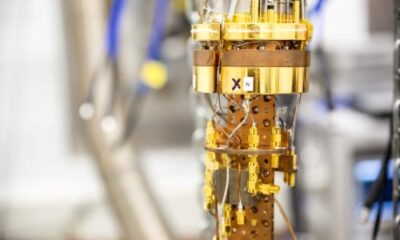
 Science2 months ago
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 Top Stories2 months ago
Top Stories2 months agoDirecTV to Launch AI-Driven Ads with User Likenesses in 2026
-

 Entertainment2 months ago
Entertainment2 months agoFreeport Art Gallery Transforms Waste into Creative Masterpieces
-
 Health2 months ago
Health2 months agoGavin Newsom Critiques Trump’s Health and National Guard Plans
-

 Business2 months ago
Business2 months agoUS Government Denies Coal Lease Bid, Impacting Industry Revival Efforts