Science
Advancements in NSCLC Management: A Shift to Protein Biomarkers

The management of non-small cell lung cancer (NSCLC) is evolving significantly, as recent discussions at the 20th Annual New York Lung Cancers Symposium revealed a shift towards protein-based biomarkers. This change is largely driven by the approval of innovative therapies, particularly antibody-drug conjugates (ADCs), and a deeper understanding of therapeutic resistance. Dr. Soo-Ryum Yang, an assistant attending pathologist at Memorial Sloan Kettering Cancer Center, outlined these developments during his presentation on November 15, 2025.
Key Trends in Biomarker Testing
Dr. Yang highlighted four major trends influencing NSCLC management: the rise of protein-based immunohistochemistry (IHC) biomarkers for ADCs, the actionability of tumor suppressor genes, the therapeutic potential of synthetic lethality, and advancements in computational pathology. He emphasized the pressing issue of tissue scarcity, which complicates the implementation of multiplex IHC and broad panel next-generation sequencing (NGS). These methods are crucial for delivering personalized therapies to a wider range of NSCLC patients.
Pathologists are increasingly focusing on the expression levels of proteins on cancer cells, which serve as actionable biomarkers. For instance, while PD-L1 IHC testing has been established for guiding checkpoint inhibitor therapy, it is now also being utilized to inform ADC treatment decisions. Dr. Yang pointed to two critical protein biomarkers in NSCLC: HER2 and c-MET. Notably, HER2 overexpression occurs in up to 20% of patients, with the highest level, classified as IHC 3+, found in around 3% of cases. Importantly, there is no direct link between HER2 mutation status and its overexpression.
The FDA recently approved fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu) for HER2-positive solid tumors, including NSCLC patients who have undergone prior treatment. This approval was bolstered by the findings from the phase 2 DESTINY-Lung01 study, which utilized HER2 scoring guidelines originally established for gastric cancer. Dr. Yang advocated for the application of these guidelines in NSCLC testing.
Similarly, c-MET overexpression is prevalent in NSCLC, with an actionable c-MET-high status found in approximately 17% of EGFR wild-type cases. The FDA granted accelerated approval to telisotuzumab vedotin-tllv (teliso-V; Emrelis) for this patient group, based on data from the phase 2 LUMINOSITY trial.
Challenges and Future Directions
Integrating HER2 and c-MET IHC screening into existing diagnostic frameworks poses significant challenges. Dr. Yang proposed a flexible approach to diagnostics, recommending standardized options that allow institutions to develop optimized workflows based on their specific resources and multidisciplinary input.
Several promising biomarkers are being investigated for their potential to become standard in NSCLC treatment. Dr. Yang noted that KRAS mutations occur in up to 40% of lung adenocarcinomas, with various mutations, including KRAS G12C, G12V, and G12D, presenting different clinical challenges. Notably, the KRAS G12D mutation is often associated with a history of light or non-smoking and correlates with poorer response rates to chemoimmunotherapy.
Established therapies targeting KRAS G12C, such as sotorasib (Lumakras) and adagrasib (Krazati), are now complemented by ongoing clinical trials exploring treatments for other KRAS mutations. For example, zoldonrasib (RMC-9805), a KRAS G12D inhibitor, demonstrated an overall response rate of 61% in early studies.
Dr. Yang also discussed the significance of tumor suppressor gene mutations, particularly in STK11 and KEAP1, which impact up to 20% of lung cancers. These mutations contribute to an immunosuppressive tumor microenvironment, making them potential biomarkers for escalating checkpoint therapy. Data from the phase 3 POSEIDON trial suggests that combining CTLA-4 inhibitors with PD-L1 inhibitors and chemotherapy may offer a strategy to overcome resistance in patients with these mutations.
The discussion also touched on MTAP deletions, which occur in about 18% of lung cancers. These deletions create a metabolic vulnerability that can be targeted through synthetic lethality. Detection methods for MTAP include NGS, which is sensitive to tumor purity, and IHC, which can identify protein expression loss.
As the landscape of NSCLC management broadens, Dr. Yang emphasized the need for comprehensive biomarker testing incorporating both protein analysis and computational insights. The advent of AI-driven methodologies, such as the quantitative scoring of TROP2 expression in ADC trials, represents a significant advancement. Although preliminary results are promising, further validation is necessary to enhance predictive power and ensure accessibility across diagnostic platforms.
In conclusion, the field of NSCLC management is transitioning from a focus solely on genomics to a more multifaceted approach that includes protein biomarkers and innovative therapeutic strategies. Dr. Yang believes that in the coming years, broad-panel NGS, IHC, and AI will be integral to advancing personalized medicine for a larger segment of the lung cancer population.
-

 Top Stories1 month ago
Top Stories1 month agoNew ‘Star Trek: Voyager’ Game Demo Released, Players Test Limits
-

 World1 month ago
World1 month agoGlobal Air Forces Ranked by Annual Defense Budgets in 2025
-

 World1 month ago
World1 month agoMass Production of F-35 Fighter Jet Drives Down Costs
-
 World1 month ago
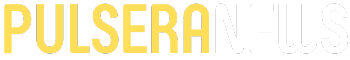
World1 month agoElectrification Challenges Demand Advanced Multiphysics Modeling
-
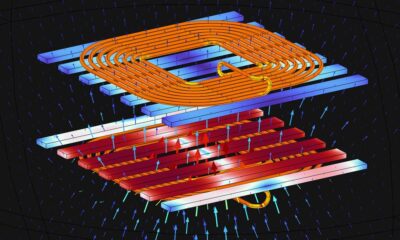
 Science1 month ago
Science1 month agoTime Crystals Revolutionize Quantum Computing Potential
-

 Business1 month ago
Business1 month agoGold Investment Surge: Top Mutual Funds and ETF Alternatives
-

 Entertainment1 month ago
Entertainment1 month agoFreeport Art Gallery Transforms Waste into Creative Masterpieces
-

 Top Stories1 month ago
Top Stories1 month agoDirecTV to Launch AI-Driven Ads with User Likenesses in 2026
-

 Lifestyle4 weeks ago
Lifestyle4 weeks agoDiscover Reese Witherspoon’s Chic Dining Room Style for Under $25
-
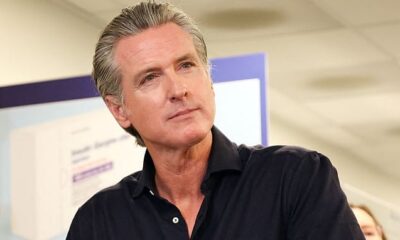
 Health4 weeks ago
Health4 weeks agoGavin Newsom Critiques Trump’s Health and National Guard Plans
-

 Business1 month ago
Business1 month agoUS Government Denies Coal Lease Bid, Impacting Industry Revival Efforts
-

 Lifestyle1 month ago
Lifestyle1 month agoLia Thomas Honored with ‘Voice of Inspiration’ Award at Dodgers Event