Health
Promising Phase 2 Trial Shows BNT111 Enhances Melanoma Treatment
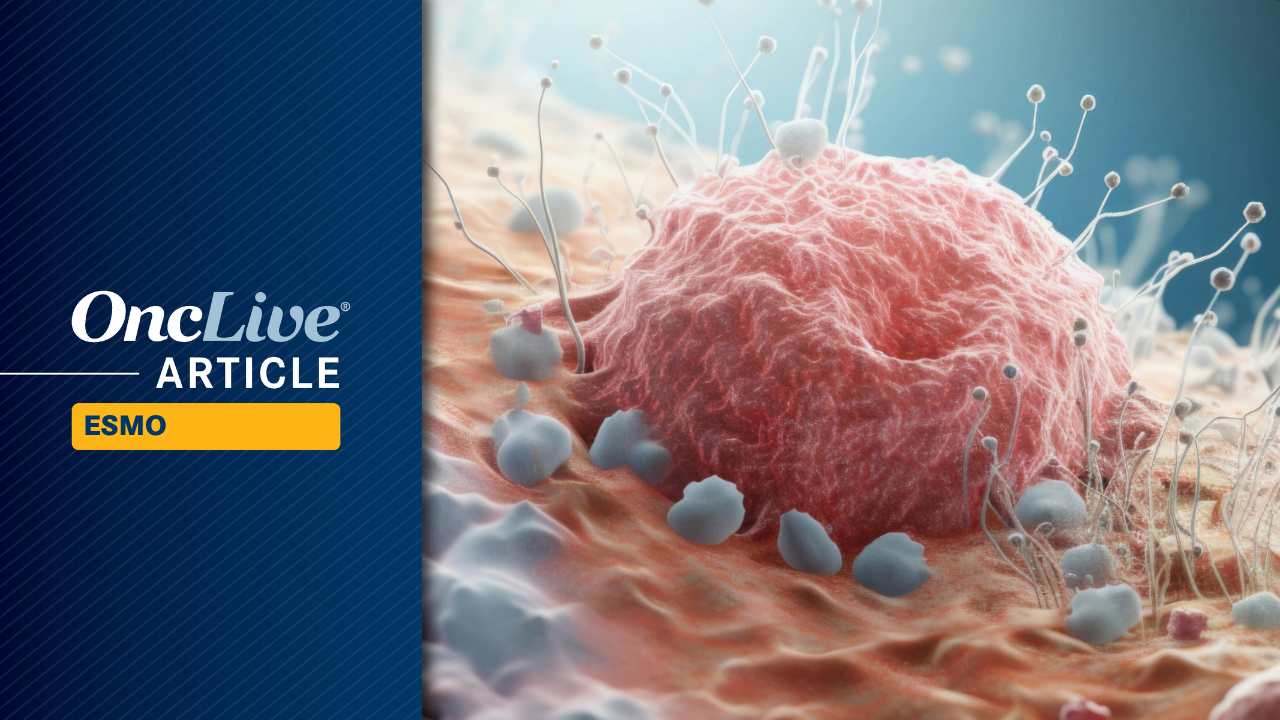
New data from the Phase 2 trial of BNT111 in combination with cemiplimab (Libtayo) has revealed an objective response rate (ORR) of 18.1% in patients with PD-(L)1-relapsed/refractory melanoma. This finding allows researchers to reject the null hypothesis suggesting an ORR below 10%. The results were presented at the 2025 ESMO Congress and highlight the potential of this treatment in a challenging patient population.
The Phase 2 BNT111-01 trial (NCT04526899) demonstrated significant efficacy, where the best responses included a complete response (CR) rate of 11.7%, a partial response (PR) rate of 6.4%, and a stable disease (SD) rate of 37.2%. Overall, the disease control rate (DCR) was 55.3%, suggesting that the combination therapy is effective for many patients who have limited treatment options.
With a median follow-up of 15.7 months, the median progression-free survival (PFS) was recorded at 3.1 months, with a 24-month PFS rate of 24.9%. Furthermore, the median overall survival (OS) reached 20.7 months, with 47.8% of patients surviving at the 24-month mark. Lead study author Paolo Ascierto, MD, a full professor of oncology at the University of Napoli Federico II and director of the Department of Melanoma at the Istituto Nazionale Tumori IRCCS Fondazione Pascale, noted the statistically significant improvement of BNT111 plus cemiplimab compared to an assumed historical ORR of 10%.
BNT111 is an investigational cancer immunotherapy that utilizes uridine RNA-based lipoplex technology to target nonmutated tumor-associated antigens. The trial was designed as an open-label, randomized, multi-center study to evaluate the safety and activity of BNT111 in combination with cemiplimab as a second-line therapy for patients with unresectable stage III or IV melanoma who had previously progressed on PD-(L)1 therapy.
To qualify for the trial, patients had to have measurable disease, serum lactate dehydrogenase levels below the upper limit of normal, and had to have received up to five prior lines of therapy, including ipilimumab (Yervoy). Most participants entered the trial within six months of confirmed disease progression and had undergone at least 12 weeks of treatment that included a BRAF-based combination for those with BRAF-mutant disease.
A total of 180 patients were randomly assigned to one of three treatment arms: BNT111 plus cemiplimab (94 patients), BNT111 monotherapy (46 patients), or cemiplimab monotherapy (44 patients). Each treatment was administered for up to 24 months, and patients in the monotherapy arms were permitted to add the other agent upon confirmation of disease progression.
The primary endpoint was the ORR by blinded independent central review per RECIST 1.1 in the combination group, which was compared with the historical control ORR of 10%. Secondary endpoints included ORR in monotherapy arms, duration of response, DCR, time to response, PFS, OS, safety, tolerability, and patient-reported outcomes. Safety was monitored for 90 days, and overall survival was assessed every three months for up to 48 months.
Baseline characteristics of the combination arm revealed a median age of 64.0 years, with a majority of participants being male (63.8%) and having an Eastern Cooperative Oncology Group (ECOG) performance status of 0 (78.7%). Most patients (97.9%) had stage IV disease, and 56.4% had received multiple prior therapies. Notably, 56.4% were PD-(L)1 refractory, and 25.5% presented with liver metastases.
Ascierto emphasized that all patients were PD-(L)1 relapsed/refractory and had undergone previous treatments, with half of them having been pretreated with CTLA4. He also highlighted that BNT111 demonstrated clinical activity as a monotherapy, yielding an ORR of 17.4% with best responses including a CR rate of 13.0%.
In the cemiplimab monotherapy arm, the ORR was reported at 13.6%, with a median OS of 22.3 months. The safety profile for the combination therapy was deemed manageable, with treatment-emergent adverse effects (TEAEs) related to cytokine release, including pyrexia (76.1%), hypertension (12.0%), and chills (51.1%).
In conclusion, Ascierto stated, “BNT111, both as a monotherapy and in combination therapy, exhibited a manageable safety profile, primarily driven by the induction of cytokines through toll-like receptors by the single-stranded RNA immunotherapy.”
The positive topline results were initially announced in July 2024, following the fast track designation from the FDA for BNT111 as a potential treatment for advanced melanoma.
-
 Science3 months ago
Science3 months agoALMA Discovers Companion Orbiting Giant Red Star π 1 Gruis
-

 Science3 months ago
Science3 months agoDoctoral Candidate Trivanni Yadav Advances Battery Research at UTulsa
-

 World4 months ago
World4 months agoGlobal Air Forces Ranked by Annual Defense Budgets in 2025
-

 Top Stories4 months ago
Top Stories4 months agoNew ‘Star Trek: Voyager’ Game Demo Released, Players Test Limits
-

 World4 months ago
World4 months agoMass Production of F-35 Fighter Jet Drives Down Costs
-
 Sports3 months ago
Sports3 months agoNASCAR Faces Fan Backlash as Steve Phelps’ Texts Surface
-

 Business4 months ago
Business4 months agoGold Investment Surge: Top Mutual Funds and ETF Alternatives
-

 Top Stories4 months ago
Top Stories4 months agoDirecTV to Launch AI-Driven Ads with User Likenesses in 2026
-

 Politics4 months ago
Politics4 months agoSEVENTEEN’s Mingyu Faces Backlash Over Alcohol Incident at Concert
-
 Science4 months ago
Science4 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 Entertainment4 months ago
Entertainment4 months agoFreeport Art Gallery Transforms Waste into Creative Masterpieces
-

 Science4 months ago
Science4 months agoRemembering David E. Brest: A Life Dedicated to Nature and Family