Health
Stanford Study Reveals Mechanisms Behind COVID-19 Vaccine Myocarditis

A recent study from Stanford University has provided new insights into myocarditis, a rare but notable side effect associated with COVID-19 vaccinations, particularly affecting young males. The research indicates that two specific proteins, CXCL10 and IFN-gamma, released by immune cells, play a significant role in causing heart inflammation following vaccination.
Myocarditis, which is characterized by inflammation of the heart muscle, has been reported in approximately one in 140,000 individuals after receiving the first vaccine dose and one in 32,000 following the second. The incidence rate escalates for males aged 30 and younger, with estimates at one in 16,750. Symptoms typically manifest within one to three days post-vaccination and include chest pain, shortness of breath, fever, and palpitations. Elevated levels of cardiac troponin, a marker for heart muscle damage, often accompany these symptoms.
Joseph Wu, MD, PhD, who leads the Stanford Cardiovascular Institute, emphasized that while myocarditis can be serious, most patients recover quickly without lasting heart damage. “It’s not a heart attack in the traditional sense,” Wu explained. “There’s no blockage of blood vessels as found in most common heart attacks. When symptoms are mild and inflammation hasn’t caused structural damage, we simply observe these patients to ensure they recover.”
The study, conducted in collaboration with The Ohio State University, aimed to elucidate the underlying mechanisms of vaccine-related myocarditis. Researchers analyzed blood samples from vaccinated individuals, comparing those with myocarditis to those without. Their findings revealed that increased levels of CXCL10 and IFN-gamma were present in the blood of those experiencing myocarditis, suggesting these proteins may drive the inflammation process.
“We believe these two are the major drivers of myocarditis,” Wu stated. “Your body requires these cytokines to combat viruses. They are essential for immune response, but in excessive amounts, they can become toxic.” Animal models and heart tissue studies showed that elevated levels of these proteins correlate with signs of heart irritation, akin to mild myocarditis.
In an encouraging development, the research team discovered that blocking the action of these cytokines significantly reduced heart damage in their models. “One of the most striking findings was how much we could lessen heart damage by specifically targeting these two cytokines without compromising the overall immune response to the vaccine,” Wu noted. This suggests a potential strategy for preventing or treating myocarditis in individuals at higher risk while still reaping the benefits of vaccination.
The study also explored the effects of genistein, a natural compound resembling estrogen and found in soybeans, which demonstrated an ability to reduce inflammation in laboratory settings. However, its efficacy in humans has yet to be evaluated.
These findings were published in the journal Science Translational Medicine. Dr. Marc Siegel, a senior medical analyst, commented, “Myocarditis is very rare, and the immune mechanism makes sense.” Wu further clarified that the risk of myocarditis following a COVID-19 infection is approximately ten times greater than the risk associated with mRNA vaccines.
Despite these findings, the researchers highlighted the well-established safety record of COVID-19 vaccines. “mRNA vaccines remain a crucial tool against COVID-19,” Wu affirmed. “This research helps explain a rare side effect and suggests ways to make future vaccines even safer, rather than serving as a deterrent to vaccination. The overall benefits of COVID-19 vaccination still clearly outweigh the small risk of myocarditis for nearly all groups.”
While the study provides valuable insights, Wu acknowledged its limitations, particularly the reliance on experimental systems that may not fully replicate how myocarditis develops and resolves in real-world patients. “This points to a possible future way to prevent or treat myocarditis in those at the highest risk,” he said, emphasizing the need for clinical studies to confirm the safety and effectiveness of targeted treatments.
He also noted that myocarditis can occur with other vaccines, though the symptoms are often less specific. “Other vaccines can cause myocarditis and inflammatory problems, but the symptoms tend to be more diffuse,” he explained. The heightened scrutiny and media coverage surrounding mRNA COVID-19 vaccines have led to increased awareness and reporting of myocarditis cases.
The study received funding from the National Institutes of Health and the Gootter-Jensen Foundation, underscoring the commitment to understanding vaccine side effects and improving public health outcomes.
-
 Science1 month ago
Science1 month agoALMA Discovers Companion Orbiting Giant Red Star π 1 Gruis
-

 Politics2 months ago
Politics2 months agoSEVENTEEN’s Mingyu Faces Backlash Over Alcohol Incident at Concert
-

 Top Stories2 months ago
Top Stories2 months agoNew ‘Star Trek: Voyager’ Game Demo Released, Players Test Limits
-

 World2 months ago
World2 months agoGlobal Air Forces Ranked by Annual Defense Budgets in 2025
-

 World2 months ago
World2 months agoMass Production of F-35 Fighter Jet Drives Down Costs
-
 World2 months ago
World2 months agoElectrification Challenges Demand Advanced Multiphysics Modeling
-

 Business2 months ago
Business2 months agoGold Investment Surge: Top Mutual Funds and ETF Alternatives
-
 Science2 months ago
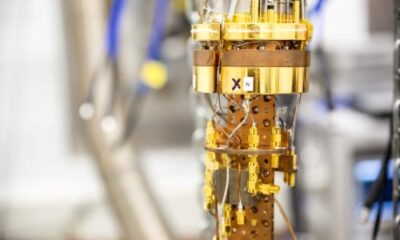
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 Top Stories2 months ago
Top Stories2 months agoDirecTV to Launch AI-Driven Ads with User Likenesses in 2026
-

 Entertainment2 months ago
Entertainment2 months agoFreeport Art Gallery Transforms Waste into Creative Masterpieces
-

 Business2 months ago
Business2 months agoUS Government Denies Coal Lease Bid, Impacting Industry Revival Efforts
-
 Health2 months ago
Health2 months agoGavin Newsom Critiques Trump’s Health and National Guard Plans