Health
Study Reveals 92% of Dementia Patients Face Burdensome Care Interventions

A comprehensive study conducted by researchers from Duke-NUS Medical School has found that over 90% of older adults with advanced dementia in Singapore undergo at least one burdensome medical intervention during their final year of life. This research underscores an urgent need for improved strategies to support families and reduce unnecessary medical procedures at the end of life.
The study, published in the Journal of Gerontology: Medical Sciences, examined the care experiences of community-dwelling older adults with dementia in Singapore. It highlights that 92% of these individuals experienced interventions such as feeding tubes or physical restraints, which experts argue do not enhance comfort or survival rates. As the number of people living with dementia in the Asia-Pacific region is expected to reach 71 million by 2050, these findings are particularly significant, given that most previous research on the topic has been based in Western contexts.
Key Findings on End-of-Life Care
The research identified several critical issues affecting the quality of end-of-life care for older adults with dementia living at home. The data was collected from the longitudinal cohort study, titled PISCES (Panel study Investigating Status of Cognitively impaired Elderly in Singapore), in which family caregivers were surveyed every four months between 2018 and 2023.
One of the main issues highlighted was the overreliance on burdensome medical interventions. Almost all participants experienced taxing treatments in their final year, with 49% receiving antibiotics, 22% receiving intravenous fluids, and 74% subjected to feeding tubes or restraints. The rate of tube feeding was notably higher than in Western studies, often leading to the use of physical restraints to prevent tube removal. Experts recommend careful hand feeding over tube feeding due to the associated risks.
Hospitalization rates among older adults with dementia were also alarming, with nearly half (48%) being hospitalized for at least one night in their final year. Furthermore, 35% died in hospital, a significant increase compared to Western studies where nursing homes are the primary place of death. Such increased hospitalizations can expose patients to stressful and costly care experiences with little clinical benefit.
Impact on Caregivers and the Need for Support
The burden on informal caregivers is profound, with 42% of family members providing at least 60% of total care for their loved ones. Many caregivers are forced to quit their jobs, with 30% reporting job loss due to caregiving responsibilities. On average, caregivers dedicate 42 hours per week to provide care, which translates to an estimated annual wage of S$32,125.
Despite the heavy burden, caregivers reported feeling inadequately supported. A significant 62% indicated they received insufficient information when making care decisions, and only 15% were informed about their loved ones’ life expectancy. This highlights a critical gap in communication and support for caregivers during a challenging time.
Dr. Ellie Bostwick Andres, first author of the study and a senior research fellow at the Lien Center for Palliative Care at Duke-NUS, emphasized the disconnect between caregivers’ values and the actual experiences of older adults. She noted, “Frequent hospitalizations and the widespread use of interventions generally deemed ‘low-value’ among older adults living at home highlight the need to adopt a palliative approach at home to alleviate symptoms and minimize burden on older adults and their caregivers.”
Dr. Chetna Malhotra, senior author and Research Director at the Lien Center, added that cultural values in Asia influence caregiving approaches. Families often feel compelled to prolong life rather than consider palliative options. Consequently, educational strategies promoting palliative care must be tailored to regional cultural contexts.
Insights from this study are being utilized to develop tools that support caregivers, such as CareBuddy, a mobile application designed to promote healthy aging, alongside decision aids to facilitate informed care choices.
Professor Patrick Tan, Dean-designate and Senior Vice-Dean for Research at Duke-NUS, remarked on the human aspect of dementia care in Asia, stating, “These findings reveal the human reality of dementia care—one defined by love, sacrifice, and difficult choices. As more older adults spend their final days at home, it’s critical that we build systems of care that show compassion not only to patients but also to their caregivers who sustain them.”
The study serves as a call to action for policymakers and healthcare providers to reevaluate current practices and enhance support systems for both patients and caregivers in the face of an aging population.
-

 Top Stories1 month ago
Top Stories1 month agoNew ‘Star Trek: Voyager’ Game Demo Released, Players Test Limits
-

 World1 month ago
World1 month agoGlobal Air Forces Ranked by Annual Defense Budgets in 2025
-

 World1 month ago
World1 month agoMass Production of F-35 Fighter Jet Drives Down Costs
-
 World1 month ago
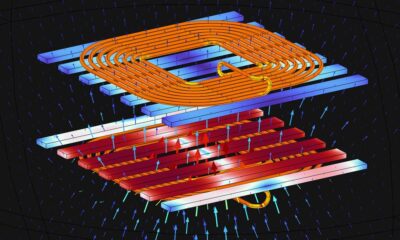
World1 month agoElectrification Challenges Demand Advanced Multiphysics Modeling
-
 Science1 month ago
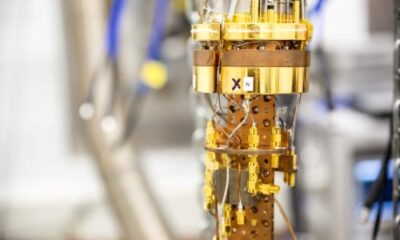
Science1 month agoTime Crystals Revolutionize Quantum Computing Potential
-

 Business1 month ago
Business1 month agoGold Investment Surge: Top Mutual Funds and ETF Alternatives
-

 Entertainment1 month ago
Entertainment1 month agoFreeport Art Gallery Transforms Waste into Creative Masterpieces
-

 Top Stories1 month ago
Top Stories1 month agoDirecTV to Launch AI-Driven Ads with User Likenesses in 2026
-

 Lifestyle1 month ago
Lifestyle1 month agoDiscover Reese Witherspoon’s Chic Dining Room Style for Under $25
-
 Health1 month ago
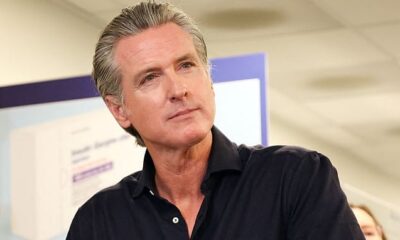
Health1 month agoGavin Newsom Critiques Trump’s Health and National Guard Plans
-

 Business1 month ago
Business1 month agoUS Government Denies Coal Lease Bid, Impacting Industry Revival Efforts
-

 Science1 month ago
Science1 month agoRemembering David E. Brest: A Life Dedicated to Nature and Family