Health
Obesity-Linked Nutrient Deficiency Threatens Young Brain Health
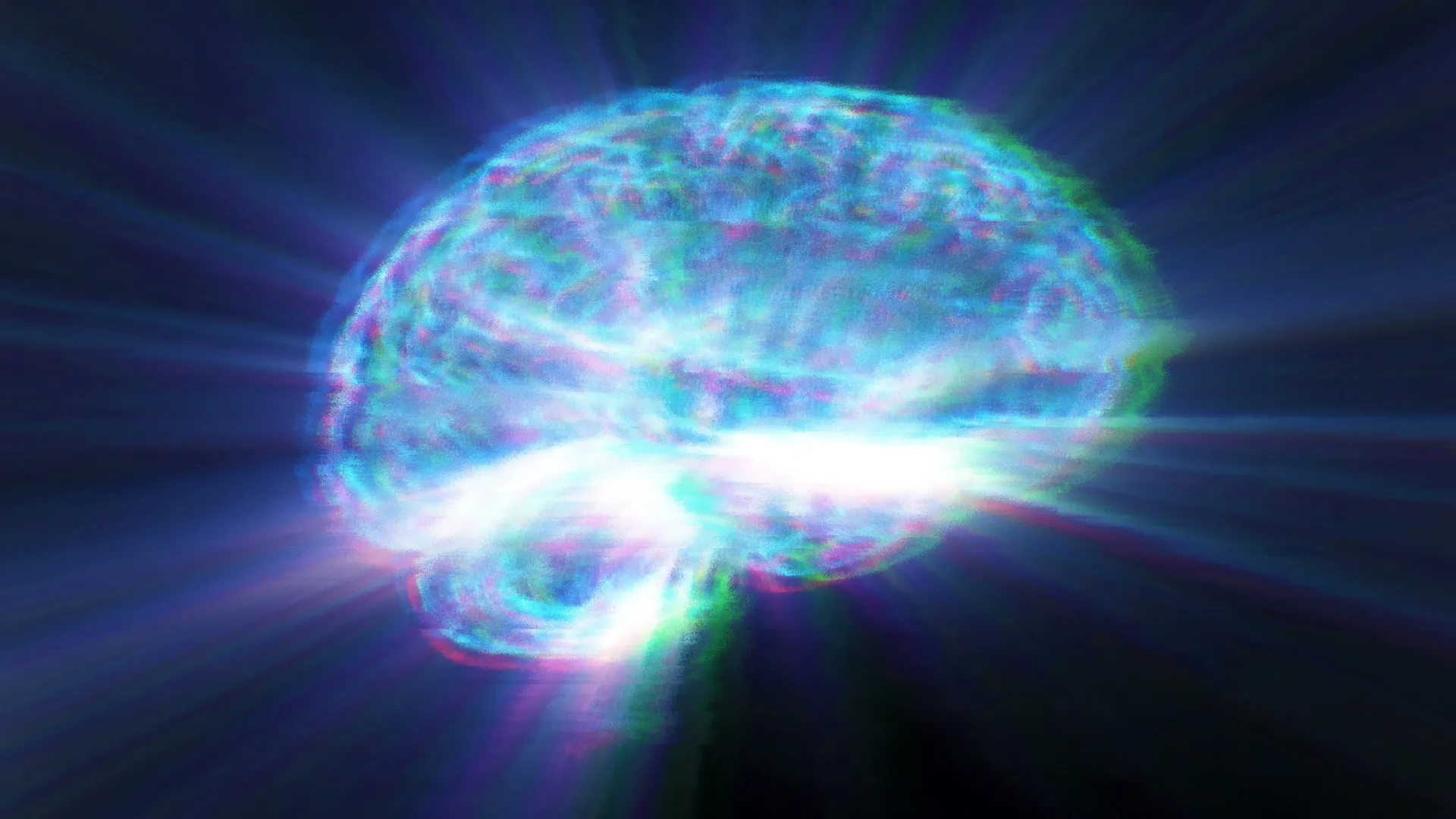
Research from Arizona State University has revealed that a common nutrient deficiency may significantly impact the brain health of young adults struggling with obesity. Findings suggest that low levels of choline—a nutrient vital for cognitive function—correlate with biological markers indicating early signs of brain stress and cognitive impairment.
In a study published on November 27, 2025, scientists focused on young adults with obesity, discovering elevated inflammation, signs of liver strain, and increased levels of neurofilament light chain (NfL), an indicator of neuronal injury. The research highlights that these changes often precede noticeable cognitive symptoms, hinting at early metabolic disruptions affecting brain health.
Link Between Obesity and Brain Function
Traditionally, obesity has been linked to various chronic health conditions, such as heart disease and type 2 diabetes. However, this study underscores that the negative effects on brain function may manifest sooner than previously thought. The researchers identified troubling patterns in young adults, including increased levels of inflammation-promoting proteins and enzymes indicative of liver stress.
An important discovery was the unusually low blood levels of choline among these participants. Ramon Velazquez, the lead researcher from the ASU-Banner Neurodegenerative Disease Research Center, stated, “This research adds to the growing evidence that choline is a valuable marker of metabolic and brain dysfunction.” He emphasized the necessity of adequate daily choline intake for maintaining human health.
In this study, the correlation between low choline levels and increased NfL in young adults is particularly concerning. NfL levels are typically elevated in individuals with mild cognitive impairment and Alzheimer’s disease, making these findings significant, as they suggest that obesity could have detrimental effects on the brain long before symptoms appear.
The Role of Choline in Brain and Metabolic Health
Choline is essential for various bodily functions, including cell-membrane structure, inflammation regulation, and liver function. It also plays a critical role in the production of acetylcholine, a neurotransmitter crucial for memory and cognitive processes. Participants in the study exhibited significantly lower circulating choline levels, which were linked to stronger indicators of inflammation, insulin resistance, and neuronal damage.
While some choline is produced by the liver, the majority must be obtained through diet. Rich sources include eggs, poultry, fish, beans, and cruciferous vegetables like broccoli and cauliflower. Notably, the study found that women had lower choline levels than men, which is particularly relevant given the higher rates of cognitive aging and Alzheimer’s disease observed in women.
Data from national nutrition surveys indicate that many individuals, particularly teenagers and young adults, do not meet the recommended daily intake of choline. The lack of this nutrient may increase vulnerability to metabolic stress and exacerbate the impact of obesity on cognitive health.
Wendy Winslow, the first co-author of the study, pointed out, “Most people don’t realize they aren’t getting enough choline. Adding choline-rich foods to your routine can help reduce inflammation and support both your body and brain as you age.”
The research also raises concerns about modern weight-loss medications, which suppress appetite and may lead to insufficient intake of choline and other essential nutrients. The authors stress the importance of future studies to determine whether combining GLP-1 therapies with adequate dietary choline can help maintain metabolic resilience and overall health.
The study involved 30 adults in their 20s and 30s, evenly divided between those with obesity and those of healthy weight. Each participant provided fasting blood samples for analysis, revealing consistent patterns of lower choline levels and greater inflammation among those with obesity.
By comparing their findings with data from older adults diagnosed with mild cognitive impairment or Alzheimer’s disease, the researchers observed similar patterns of low choline and high NfL in both groups. This suggests that biological changes associated with cognitive decline may begin years before symptoms become evident, particularly in individuals experiencing obesity and metabolic stress.
In conclusion, this study reinforces the connection between obesity, inflammation, choline deficiency, and early neuronal stress. While it does not establish direct causation, it highlights a set of biomarkers resembling those found in older adults with cognitive impairment. The implications of these findings could be significant, as ongoing research aims to understand how early metabolic stress could influence long-term risks for neurodegenerative diseases, potentially leading to new strategies for promoting brain health throughout life.
-

 Top Stories2 months ago
Top Stories2 months agoNew ‘Star Trek: Voyager’ Game Demo Released, Players Test Limits
-

 World2 months ago
World2 months agoGlobal Air Forces Ranked by Annual Defense Budgets in 2025
-
 Science2 weeks ago
Science2 weeks agoALMA Discovers Companion Orbiting Giant Red Star π 1 Gruis
-

 World2 months ago
World2 months agoMass Production of F-35 Fighter Jet Drives Down Costs
-
 World2 months ago
World2 months agoElectrification Challenges Demand Advanced Multiphysics Modeling
-

 Business2 months ago
Business2 months agoGold Investment Surge: Top Mutual Funds and ETF Alternatives
-
 Science2 months ago
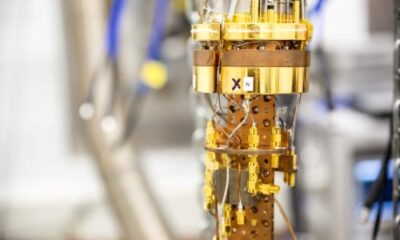
Science2 months agoTime Crystals Revolutionize Quantum Computing Potential
-

 Top Stories2 months ago
Top Stories2 months agoDirecTV to Launch AI-Driven Ads with User Likenesses in 2026
-

 Entertainment2 months ago
Entertainment2 months agoFreeport Art Gallery Transforms Waste into Creative Masterpieces
-

 Business2 months ago
Business2 months agoUS Government Denies Coal Lease Bid, Impacting Industry Revival Efforts
-
 Health1 month ago
Health1 month agoGavin Newsom Critiques Trump’s Health and National Guard Plans
-

 Lifestyle1 month ago
Lifestyle1 month agoDiscover Reese Witherspoon’s Chic Dining Room Style for Under $25